Occupations:
Activities:
Causes of Foot Disorders:

Palpation of the medial calcaneal tubercle usually elicits pain in patients presenting with plantar fasciitis.
The plantar fascia is actually a thick, fibrous band of connective tissue which originates at the heel bone and runs along the bottom of the foot in a fan-like manner, attaching to the base of each of the toes. A rather tough, resilient structure, the plantar fascia takes on a number of critical functions during running and walking. It stabilizes the metatarsal joints (the joints associated with the long bones of the foot) during impact with the ground, acts as a shock absorber for the entire leg, and helps to lift the longi-tudinal arch of the foot to prepare it for the ‘take-off’ phase of the gait cycle
Although the fascia is invested with countless sturdy ‘cables’ of connective tissue called collagen fibres, it is certainly not immune to injury. Plantar fasciitis, the most common cause of heel pain, may have several different clinical presentations. Although pain may occur along the entire course of the plantar fascia, it is usually limited to the inferior medial aspect of the calcaneus, at the medial process of the calcaneal tubercle. Often tend to occur near the heel, where stress on the connective tissue fibres is greatest, and where the fascia itself is the thinnest (it tends to broaden out as it reaches toward the toes). This bony prominence serves as the point of origin of the anatomic central band of the plantar fascia and the abductor hallucis, flexor digitorum brevis and abductor digiti minimi muscles.
Plantar fasciitis is often referred to as “heel spur syndrome” in the literature and the medical community, but the label is a misnomer. This vague and nonspecific term incorrectly suggests that osseous “spurs” (inferior calcaneal exostoses) are the cause of pain rather than an incidental radiographic finding. There is no correlation between pain and the presence or absence of exostoses,1 and excision of a spur is not part of the usual surgery for plantar fasciitis.2 Plantar fasciitis occurs in both men and women, but is more common in the latter. Its incidence and severity correlate strongly with obesity.
Plantar Fasciitis often leads to heel pain, heel spurs, and/or arch pain. The excessive stretching of the plantar fascia that leads to the inflammation and discomfort can be caused by the following:
Most cases of plantar fasciitis are the result of a biomechanical fault that causes abnormal pronation. This pronation significantly increases tension on the plantar fascia.
Other conditions, such as bowed shins, tight calves, and limb length inequality, can cause an abnormal pronatory force on the long limb. Increased pronation with a collapse produces additional stress on the anatomic central band of the plantar fascia and may ultimately lead to plantar fasciitis.
Symptoms
Patients usually describe pain in the heel on taking the first several steps in the morning, with the symptoms lessening as walking continues. They frequently relate that the pain is localized to an area that the examiner identifies as the medial calcaneal tubercle. The pain is usually insidious, with no history of acute trauma. Many patients state that they believe the condition to be the result of a stone bruise or a recent increase in daily activity. It is not unusual for a patient to endure the symptoms and try to relieve them with home remedies for many years before seeking medical treatment.
Diagnosis
Even in this age of modern technology, the diagnosis of plantar fasciitis is based mainly on the medical history and clinical presentation. Direct palpation of the medial calcaneal tubercle often causes severe pain (see Figure above). The pain is generally localized at the origin of the anatomic central band of the plantar fascia, with no significant pain on compression of the calcaneus from a medial to a lateral direction. Standard weight-bearing radiographs may show other osseous abnormalities such as fractures, tumors or rheumatoid arthritis in the calcaneus. However, radiographs usually serve only as an aid to confirm the clinician’s diagnosis.
Conservative Treatment
Conservative treatment of plantar fasciitis should address the inflammatory component that causes the discomfort and the biomechanical factors that produce the disorder. Patients should learn about recommended changes in daily activities, such as wearing appropriate shoes with a significant medial arch while walking. Patients whose symptoms are associated with a recent increase in exercise should adopt a less strenuous regimen until the plantar fasciitis resolves. An ankle/foot strengthening and stretching program will help to prevent recurrence if this is the cause.
To serve as a temporary medial arch support to decrease pronation during midstance of the gait cycle the patient can be fitted with a removable pad or a medial arch pad directly against the patient’s skin with taping the patient’s foot from a plantar medial to a plantar lateral direction that.These temporary devices provide greater biomechanical support than over-the-counter heel cups or heel pads. If a patient has significant plantar fasciitis pain secondary to a limb-length inequality a simple ¼” heel lift in the shoe of the short limb may provide temporary relief. One-sided tight calf might feel better with a bilateral heel lift.
Orthotic devices are the mainstay of ongoing conservative treatment for patients with plantar fasciitis. The biomechanical factors that cause the abnormal pronatory forces stressing the medial band of the plantar fascia must be corrected. Patients with high arched feet may benefit from using a flexible orthotic device with an additional heel cushion. This prescription orthosis can disperse some of the force experienced on heel strike, while maintaining biomechanical support for propulsion.
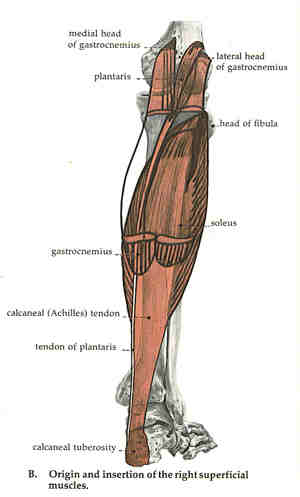
Stretching the Achilles tendon and hamstrings is beneficial as adjunctive therapy for plantar fasciitis. This can be done in conjunction with arch stretching by pulling back on the toes or rolling a can or ball back and forth under the arch. Most popular time that this is helpful is prior to rising. Seeing a massage therapist good with fascial stretching techniques can also help.
Each night for 10 to 14 days, the patient should apply an ice pack to the plantar aspect of the heel 15 to 20 minutes before going to bed.or massage the plantar fascia with an ice block (made up of water frozen in a paper cup).
It is often advantageous for patients with no contraindication to take a nonsteroidal anti-inflammatory drug (NSAID) for six to eight weeks. We believe that corticosteroid injections should be avoided in the initial treatment of plantar fasciitis; we recommend themonly as supplemental treatment in patients who have resistant chronic plantar fasciitis after achieving adequate biomechanical control. These injections may provide only temporary relief and can cause a loss of the plantar fat pad if used injudiciously.
 Night night that maintain the foot at an angle of 90 degrees or more to the ankle have recently been used as adjunctive therapy for plantar fasciitis. These orthoses prevent contraction of the plantar fascia while the patient sleeps. One study showed relief of recalcitrant plantar fasciitis pain in 83 percent of patients treated with such splints.
Night night that maintain the foot at an angle of 90 degrees or more to the ankle have recently been used as adjunctive therapy for plantar fasciitis. These orthoses prevent contraction of the plantar fascia while the patient sleeps. One study showed relief of recalcitrant plantar fasciitis pain in 83 percent of patients treated with such splints.
Shock wave or laser therapy can sometimes help to increase blood flow to stimulate the healing process.
Some clinicians advocate the use of a short-leg walking cast for several weeks as a final conservative step in the treatment of plantar fasciitis.
www.pedorthic.ca/conditions-heel
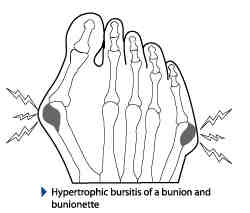 Several features combine to create the infamous bunions that are the plague of every woman who loves to wear tight fashion shoes. Like many of our physical features, bunions tend to be inherited, but get worse with time. Severe bunions can be seen even in 12 year olds, but rarely in males. In the diagram above you can see the big toe joint going out of shape with the typical large bump (subluxed joint and thickened bursa), the widened foot and the end of the toe angling inwards.
Several features combine to create the infamous bunions that are the plague of every woman who loves to wear tight fashion shoes. Like many of our physical features, bunions tend to be inherited, but get worse with time. Severe bunions can be seen even in 12 year olds, but rarely in males. In the diagram above you can see the big toe joint going out of shape with the typical large bump (subluxed joint and thickened bursa), the widened foot and the end of the toe angling inwards.
The shape of the foot however, does not usually have much to do with the pain of a bunion. Bunion pain is most often caused by the wider foot and its prominent bump rubbing against the side of the shoe. The bursa (a small, flat, fluid-filled sac that lies just below the skin on the outside of the bump), becomes inflamed and thickened. Even shoes that you once thought were loose may be tight enough to create a great deal of pain. Wearing wider shoes usually
eliminates the pain, but the bump makes fitting tight shoes very difficult.
Surgery is the only alternative to reduce the size of the bump and the hallux valgus angle. There are several different procedures which have both pros and cons . Most patients will try other methods of managing the condition initially.
Bunion formation is likely accelerated by hyperpronation (excessive lowering of the arches) because of the excessive weight placed on the big toe joint during the pushoff phase of gait, forcing the hallux into further valgus. More friction between the bursa and the shoe occurs with a hyperpronated foot. Once the hallux valgus angle is significant it destabilizes the foot during push-off since the great toe is not available for push off.
The pain of hallux rigidus (osteoarthritis of the great toe) or conditions like gout can sometimes mimic the pain of bunions so see your doctor for a proper assessment. Tight, pointed toeboxes force the hallux into greater valgus for hours at a time and should therefore be used in moderation. Shoes should be devoid of seams since stitching does not stretch easily. Pumps should be high in the vamp, covering the bunion completely, rather that the more classic style that cuts across it. Bunions that ache at night can be relieved with ice and a bunion splint that straightens the toe temporarily.
Constant use of a hallux valgus night splint may reduce the ligamentous contractures associated with long term bunions. Gel toe spreaders may also provide relief. Pre-stretch the bunion area at the shoe repair shop rather than make your foot do the work, or purchase a “ball and ring” stretcher made for that purpose. Wear a heel height that is comfortable, and wear supportive walking or running shoes with a roomy toebox whenever possible. Wear orthotics or arch supports as your doctor prescribes them to control hyperpronation.
 What is it?
What is it?Several factors
Arthritis is a disease characterized by the inflammation of the cartilage and lining of the body’s joints. Inflammation causes redness, warmth, pain and swelling. Arthritis is often considered a disease of the aging but can occur at any age. The primary targets for arthritis are people over the age of 50. Arthritis is a major cause of foot pain because each foot has 33 joints that can become affected by the disease. Arthritis causes changes in joints and restriction of motion. These changes and restrictions can make walking painful.
Arthritis is a general term for a variety of conditions that cause inflammation and degeneration of the cartilage and lining of the joints of the body. There are many different kinds of arthritis. Some of the most common types are osteoarthritis and rheumatoid arthritis. The term arthritis refers to more than 100 different rheumatic diseases that affect the joints, muscles, and bones, as well as other tissues and structures. Gout accounts for approximately 5 percent of all cases of arthritis.
Osteoarthritis is typically considered to result from normal “wear and tear” or age, but can also result from previous injury with stiffness usually occurring after periods of rest.
Rheumatoid arthritis can occur at any age and there is no known cause for this condition. It can cause severe deformities of the joints, especially in the hands and feet. It can develop at any age and there is no known cause for this condition. Rheumatoid arthritis is the most crippling form of the disease that can affect people of all ages. It can cause severe deformities of the joints with associated fatigue of the entire body. People who suffer from rheumatoid arthritis often develop severe forefoot problems such as bunions, hammer toes, claw toes, and others.
Arthritic footwear should accommodate swelling of the foot. Orthotics designed to provide comfort, support and extra cushioning are also recommended. Orthotics made with a material called Plastazote are often recommended because they mold to your feet to provide customized comfort. The proper footwear and orthotics will reduce pressure to provide a comfortable support base.
Gout is one of the most painful rheumatic diseases. Our blood contains a salt called uric acid. It results from deposits of excess needle-like crystals of uric acid in connective tissue, in the joint space between two bones, or in both. These deposits lead to inflammatory arthritis, which causes swelling, redness, heat, pain, and stiffness in the joints. The big toe joint is commonly the focal point due to the stress and pressure it experiences during walking and other weight bearing activities. This often leads to severe pain in the big toe. Up to 60% of initial attacks occur at the first metatarsophalangeal joint. Gout mostly affects men and is very rare in women until after menopause when it is seen quite often.
The signs and symptoms of gout are almost always acute, occurring suddenly – often at night – and without warning. They include Intense joint pain swelling, and redness usually affecting the large joint of your big toe but can occur in your feet, ankles, knees, hands and wrists. The pain typically lasts five to 10 days and then stops. The discomfort subsides gradually over one to two weeks, leaving the joint apparently normal and pain-free. After the first attack there may be intervals of many months or even years before there are other attacks. Over time these attacks tend to become more frequent and more severe and eventually may involve other and more joints.
There are many causes of hyperuricaemia (high uric acid levels) which include:
The crystals also have a tendency to form on a roughened surface, such as a joint that has suffered from previous trauma, unreduced subluxation, or degeneration.
In the acute and chronic stages, ultrasound, heat, gentle chiropractic manipulative therapy and gentle soft-tissue massage are beneficial.

Metatarsalgia-sesamoiditis
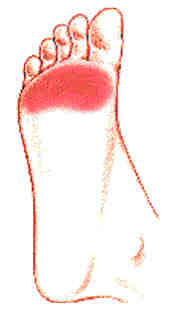 Foot pain in the “ball of your foot,” that area between your arch and the toes, is generally called metatarsalgia (met’-a-tar-sal’-gee-a). It’s a non-specific diagnosis of pain in and about the Metatarsal (MT) head or MTP (Metatarsal/Phalangeal) joint and adjacent soft tissue structures.
Foot pain in the “ball of your foot,” that area between your arch and the toes, is generally called metatarsalgia (met’-a-tar-sal’-gee-a). It’s a non-specific diagnosis of pain in and about the Metatarsal (MT) head or MTP (Metatarsal/Phalangeal) joint and adjacent soft tissue structures.
Morton’s foot (long 2nd metatarsal), Freiberg’s Disease (usually 2nd metatarsal head osteochondritis in young women), Metatarsal stress fractures (hair-line cracks that arise in bone as the result of repeated low-level forces), sesamoiditis (gradual onset of and increasing pain at the plantar aspect of the medial plantar border of the 1st MPJt (metatarsal phalangeal joint) with swelling and decreased ROM (range of motion), Morton’s neuromas (usually in heavier women, where the lateral and medial plantar nerves get compressed in the 3rd interdigital space), ganglionic cysts (weak wall of a synovial tendon sheath or jt. capsule), joint capsulitis (frequently secondary to OA (osteoarthritis) and RA(rheumatoid arthritis) or ongoing low-grade Jt. trauma), synovitis (common in RA), flexor tenosynovitis, rheumatoid bursae and nodules (those with RA tend to be very large over the bunion and plantar aspect of MPJts., and fibrinoid nodules over bony prominences), bursitis (shearing of bursa may cause it to become fibrous, distended, inflamed, infected or even calcified), transient ischaemia (nerve and artery serving the affected nerve are compressed during gait by the distal distension of the intermetatarsal bursa), gouty tophus (1st MPJt. Uric acid crystal-idposition), myalgia, neoplastic disease (rare tumours) , plantar plate rupture (from hyperextension @ 1st- turf toe) (tough, rectangular, fibrocartilaginous structure that overlies the plantar aspects of the MPJts), and focal hyperkeratosis (deep seated corns)
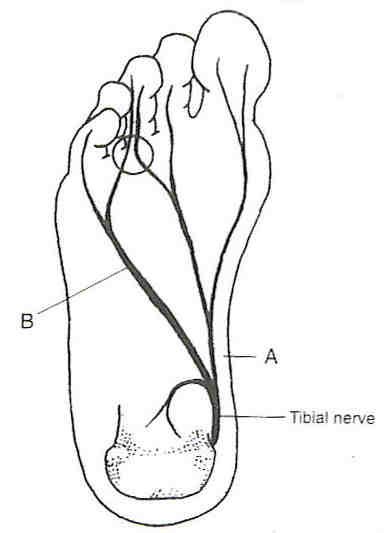
Morton’s Neuroma Site
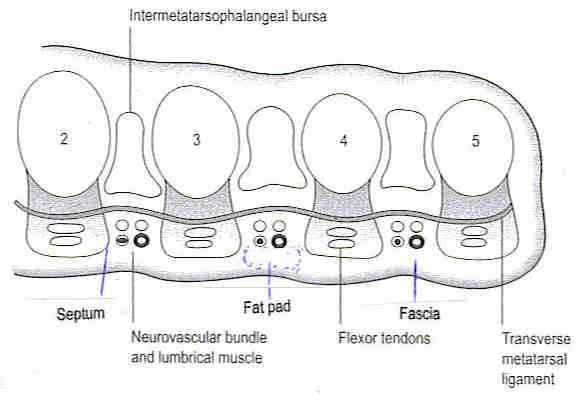
Bursitis
Posterior tibialis tendonitis is an inflammation of the tendon that runs along the inside of the ankle and attaches to the middle of the foot along the inside edge.
The posterior tibial tendon helps hold your arch up and provides support as you step off on your toes when walking. If this tendon becomes inflamed, over-stretched or torn, you may experience pain on the inner ankle and gradually lose the inner arch on the bottom of your foot, leading to flatfoot.
Inflammation may be caused by biomechanical factors such as abnormal pronation that repetitively stretches this muscle and tendon. It can also result from being overweight, or from previous trauma, inflammatory diseases such as rheumatoid arthritis, Reiter’s syndrome or psoriatic arthritis. Excessive repetitive force such as running on a banked track or road can also cause the inflammation.
Medial Tibial Stress Syndrome includes tendonitis and periosteal irritation involving the posterior tibial muscle and tendon, the flexor muscles and tendons, and other soft tissues attached to the posteromedial border of the tibia. If left untreated this has an increased risk of turning into a stress reaction and stress fracture.
Shin splints can be caused when the anterior leg muscles are stressed by running, especially on hard surfaces or extensively on the toes, or by sports that involve jumping. Wearing athletic shoes that are worn out or don’t have enough shock absorption can also cause this condition.
It is important not to try to train through the pain of shin splints. Runners should decrease mileage for about a week and avoid hills or hard surfaces. If a muscle imbalance, poor running form or flat feet are causing the problem, a long-term solution might involve a stretching and strengthening program and orthotics that support the foot and correct over-pronation. In more severe cases, ice massage, electrostimuli, heat treatments and ultra-sound might be used.